Review of Patient Matching Within a Health Information Exchange Article
The healthcare industry is making significant progress on technical interoperability, just we continue to fall short of the promise of true health information exchange. Until we tin can consistently send and receive accurate and useful patient data nationwide, we will fail to realize the documented benefits of well-executed health information exchanges: improvements in clinical decision making and patient safety, concern process improvement, and support for value-based payment.Among the remaining challenges to successful nationwide exchange is patient matching across organizational boundaries.
 The inability to consistently and accurately match patient data creates a number of problems for physicians and other healthcare providers. Providers may have an incomplete view of a patient's medical history, care may not be well coordinated, patient records may be overlaid, unnecessary testing or improper treatment may be ordered, and patient confidence may be damaged or diminished.
The inability to consistently and accurately match patient data creates a number of problems for physicians and other healthcare providers. Providers may have an incomplete view of a patient's medical history, care may not be well coordinated, patient records may be overlaid, unnecessary testing or improper treatment may be ordered, and patient confidence may be damaged or diminished.
In addition, providers may experience a number of clinical workflow inefficiencies that are costly. Those include prolonged troubleshooting to find the correct patient record, a reversion to manual telephone and fax information commutation workflows, waiting for a duplicate lab exam order, or a manual attempt to gear up a patient record match.
To address these critical patient matching and identity management issues, The Sequoia Projection, in collaboration with the Care Connectivity Consortium (CCC), has developed a framework for future growth and improvement that will shed lite on several cardinal topics:
- A example study illustrating ane organization'south inter-organizational patient matching journey from a 10% success charge per unit to a greater than 95% success rate and what we tin can larn from their experiences;
- A patient matching maturity model designed to help organizations assess their current state and provide a roadmap towards methodically improving; and
- A list of minimally acceptable patient matching practices for CIOs, CTOs and other technology leaders to adopt, if they haven't already, and implement. This list establishes a "floor" in terms of matching patients across organizational boundaries.
2018 Updates to Patient Matching Framework
Post-obit publication of the proposed framework, The Sequoia Projection convened a Patient Identity Management Workgroup, inviting members and non-members. Comprising of industry and government experts, the workgroup was charged with dispositioning public comments to develop final recommendations for improved patient identity direction in a freely usable resource for the manufacture. Over time, it is the intent of The Sequoia Project that this document is periodically updated to capture and advance cantankerous-organizational patient matching innovations.
Patient Identity Management Work Group Members: (* Denotes co-chair)
- Jamie Bennett, Healthcare Systems Specialist, JP Systems Inc., Veterans' Health Administration
- Ryan Bramble*, Senior Director of Engineering science, Chesapeake Regional Data System for our Patients (Crisp)
- Karon Casey, It Manager, Coastal Connect Health Information Commutation
- Adam Culbertson, Innovator in Residence, HIMSS
- John T. Donnelly, President, IntePro Solutions Inc.
- Zachary Gillen*, Senior Director, Care Delivery Engineering science Services, Kaiser Permanente IT
- Eric Heflin, Primary Data Officer /Chief Engineering science Officer, The Sequoia Project
- Al Jackson, Vice President of Information Management & System Functioning, Surescripts LLC
- Lesley Kadlec, MA, RHIA, CHDA, Managing director, Practice Excellence, American Health Information Management Association (AHIMA)
- Katherine Lusk, MHSM, RHIA, FAHIMA, Master Health Data Management and Exchange Officer, Children'due south Health (Dallas, Texas)
- Rebecca Madison*, Executive Director, Alaska eHealth Network
- Shelley Mannino-Marosi, Senior Director, Program Management, Michigan Health Information Network Shared Services
- Greg Mears, Md Medical Director, ZOLL
- Wendi Melgoza, RHIA, CPHI HIM Data Quality Managing director, Sutter Wellness Shared Services
- Ben Moscovitch, Director, Health Information Engineering, The Pew Charitable Trusts
- Marty Prahl, Health Information technology Consultant, Social Security Assistants
- Catherine Procknow, Software Developer, Ballsy
- Carmen Smiley, Information technology Specialist (Health Arrangement Assay), Office of Standards & Technology HHS, Part of the National Coordinator for Wellness It
Contributing Authors of A Framework for Cantankerous-Organizational Patient Identity Matching: (* Denotes co-chair)
- Lead Author: Eric Heflin, Master Technology Officer/Chief Information Officer, The Sequoia Projection
- Shan He, Medical Computer science, Intermountain Health Care/Care Connectivity Consortium
- Kevin Isbell, Executive Managing director of Health Information Exchange, Kaiser Permanente/Care Connectivity Consortium
- Andy Kling, Director of IT, Geisinger Wellness Organization/Care Connectivity Consortium
- Katherine Lusk, Chief Health Data Management and Exchange Officer, Children's Health (Dallas, Texas)
- Odysseas Pentakalos, Ph.D., CTO, SYSNET International, Inc.
- Chris Ross, Chief Information Officer, Mayo Clinic/Care Connectivity Consortium
- Seth Selkow, Director of CCC Program and HIE Engagement, Kaiser Permanente/Intendance Connectivity Consortium
- Sid Thornton, Medical Informatics, Intermountain Health Care/Care Connectivity Consortium
- Jim Younkin, Senior Managing director, Adventurous Enquiry
- Kelly Carulli, Manager, Audacious Research
- Dawn Van Dyke, Director, The Sequoia Projection (Editor)
Below is a more detailed explanation of the topics explored inside The Sequoia Project Framework for Patient Identity Direction paper:
Instance Study
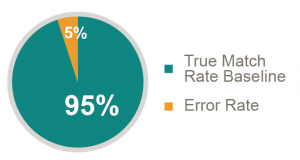
Intermountain Health Intendance, a CCC member, is a sophisticated healthcare provider and payer, and has invested heavily in healthcare information engineering science. So when they started exchanging data with other organizations, they expected a reasonably high caste of success. They surprisingly only accomplished a 10% success rate in accurately matching patient records across organizational boundaries. Through algorithmic performance and refinement, and data quality assay, Intermountain and its partners gained meaning initial improvement from 10%. Man workflow and data entry bug were next inspected, with an expected comeback to 90%, but really simply resulted in an improvement to 62%.
The remaining 38% error charge per unit was analyzed in particular and found to break down into algorithmic bug, authorization/consent issues, network and Information technology issues, and other errors such as inconsistent encoding. These improvements resulted in a match rate of 85%. A number of best practices were and so identified and implemented resulting in successful patient match rates of over 95%. These practices include systematically working with partners, addressing patient consent issues, proactively improving "fragile" identities, and addressing human workflow issues. An analysis of common patient matching traits is presented, forth with a listing of rules developed during the study. These rules are further analyzed in terms of completeness and uniqueness. The outcome was significantly improved friction match rates for Intermountain and its partners, and patient matching comeback strategies that tin be replicated across the industry.
Patient Friction match Rate Analysis
At the conclusion of the case study a number of lesson's learned and best practices are shared. There are likewise suggestions to improve cantankerous-system patient matching success to greater than 99%, which include the use of a supplemental identifier, involving the patient in the identity management process, and more than. We also provide a self-diagnostic tool, in the class of a questionnaire, to jump commencement a self-cess of your own patient matching strategies.
Patient Matching Maturity Model
Nosotros believe that more precise definitions of the maturity model will requite organizations the ability to adopt more than advanced patient identity management in a methodical manner. The levels currently being contemplated in our proposed maturity model, now open up to public comment, include:
- Level 0: Indicating ad hoc processes and outcomes, lilliputian to no management oversight or recognition;
- Level i: Indicating adoption of bones defined processes with associated repeatable outcomes, and limited management interest;
- Level ii: Indicating increasing maturation of processes, definitions of nigh key processes, information governance, algorithm use, agile management involvement, accumulation of quality metrics;
- Level 3: Indicating advanced use of existing technologies with associated management controls and senior management awareness, use of quality metrics; and
- Level four: Indicating innovation, on-going optimization, and senior direction active involvement.
Assessments are based on the International Organisation for Standardization (ISO) framework, which includes people, process, and technology, with the added dimension of governance. Current traits associated with the diverse levels include patient identity management validation plans, community collaboration, use of standards, quality metrics, knowledge sharing, partner onboarding maturity, and more. Each of these traits is defined and mapped to appropriate maturity levels.
Patient Matching Minimum Acceptable Principles
This proposed framework illustrates a very depression-level, and concrete, listing of cantankerous-organizational patient matching practices. The target audience for this, the last section in this paper, is senior technical staff responsible for implementing clinical document care summary exchange. A number of specific rules are presented, such equally the prohibition of using verbal graphic symbol-past-character matching, the corresponding responsibilities on both partners to an exchange of patient data, and like practices. Other principles include not relying on whatever specific identifier (such as a Social Security number), not making whatever assumptions about the life bicycle of a patient identifier, using normalized traits, and more.
Source: https://sequoiaproject.org/resources/patient-matching/
Post a Comment for "Review of Patient Matching Within a Health Information Exchange Article"